Five Ways to Train Smarter This Offseason
By Sean Swopes, PT, DPT, CSCS
Rausch Physical Therapy & Sports Performance
While most people take the offseason to train for a better “next year,” Mountain Bike-PT Sean Swopes explains why you should spend some time out of the saddle and try a few other methods to improve your performance and overall health.
—
You survived racing through the dirt and heat, and now the Over the Hump 2016 season has come to an end. So, what next? For many of you, the end of OTH means it’s time to pump up those skinny tires and focus on road races, crits and TT’s. Before you get back to pounding those pedals, take some time away from tuning up your bike and spend some time tuning up your body.
While the subtle differences of road cycling and mountain biking offers great balance to your riding skill level, as the quickly changing terrain and variable cadence can help to enhance your riding technique, it’s also important to spend some time out of the saddle. As a physical therapist, I know that muscle imbalance/dominance are main contributors to pain and dysfunction, but as a mountain biker I also know that many of us will go to great lengths to enhance our power output, VO2 max, and velocity.
The offseason is a great time to train to improve your performance, but it’s also the perfect time to start focusing on ways to prevent the aches and pains that may be keeping you from reaching your potential. Here are five methods you can use to stay balanced this off-season.
1. Mix Things Up
A quick and easy method I like to use to offset this imbalance is to simply go for a run. Running is a great way to change the pace and the demands of those muscle that typically get overworked when cycling. Swimming also offers a great way to continue working on aerobic demand while also decreasing the load demands on your joints.
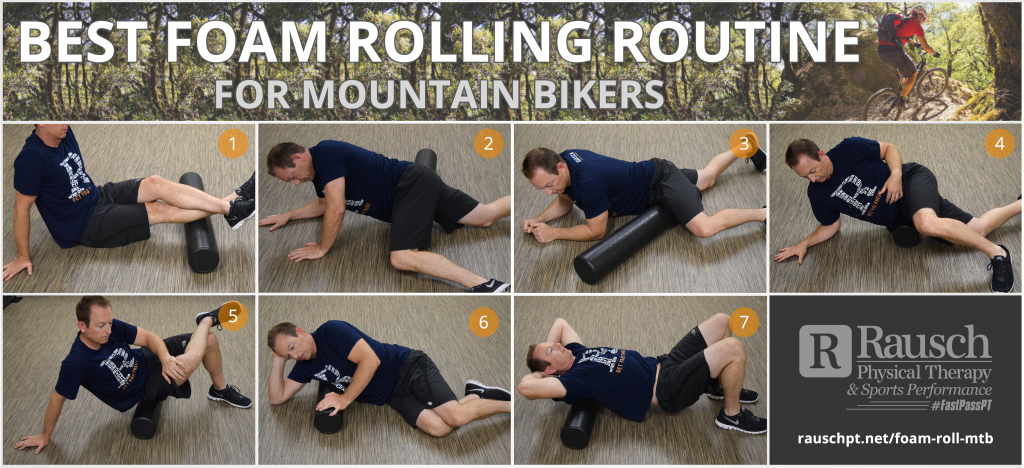
2. Get Rolling With Soft-Tissue Work
Ever feel your knees brushing the top tube during a down stroke? It’s a frequent technique used to stay in an aerodynamic position, but it can also create increased tightness of the liotibial (IT) band. In fact, it’s quite common for cyclists to develop IT Band Syndrome from repeated down stroke.
To combat this imbalance, my colleague Dustin Hancock, DPT has created a great foam rolling program to help improve flexibility and mobility of your tissues. Click here to check it out.
3. Strengthen Your Core
I went to a great workshop recently where we discussed how important it is to have core strength for successful cycling. I have been preaching this exact thing for years! We often think of our legs being our powerhouse, but how much power can you expect your legs produce without a stable base to explode from?
The primary drive for you pedal stroke is produced from the glutes, quadriceps and hamstrings. All of these muscles attach directly to the pelvis. Without good core balance and stability, your biomechanical leverage to utilize these muscle group is altered, and therefore you produce less force.
To improve your core and stability, try these exercises:
- Bird Dogs – Do these on a stable surface, or challenge yourself on an unstable surface. The key is to focus on your pelvis and prevent any rotation or tilting
- Planks – You know, that exercise we all love to do. Challenge yourself by starting with a static plank on your elbows and sides, then progress by involving leg movements.
- Swiss Ball Walkouts – Progress this exercise by incorporating knee tucks and pikes.
4. Work on Those Lungs
VO2 max is the maximum rate of oxygen consumption during vigorous activity. It’s often used to objectively measure an individual’s aerobic physical fitness and determine their endurance capacity during prolonged, submaximal exercise. The theory is: improve your VO2 max, improve your performance.
While the critical importance of VO2 max is debated, a 2012 article in the Journal of Strength and Conditioning Research concluded that VO2 max was a great determinant of mountain bike race performance, at least more so than for road races.
So, what can you do while training to improve your VO2 max? While research has shown that Hight Intensity Interval Training (HIIT) can lead to great benefits in cardiovascular gain, is HIIT really the only way to go? A 2010 article by International Journal of Sports Physiology and Performance reports that a 80/20 split in Low Intensity to High Intensity training program will create ideal physiological benefits, like V02 max.
And just remember, while it’s important to push you body to its limits to create physiological responses, this is often where injury occurs.
5. Go See a Physical Therapist
With weekly OTH races for the past three months, it’s likely you’ve developed a few aches and pains this summer. Unfortunately, many MTB racers (like most athletes) subscribe to the school of thought, “Just deal with the pain until the end of the season; it’ll get better when I stop racing.”
While I can’t force you to change your mindset, I can tell you that pain is often your body’s way of telling you that it’s undergoing an abnormal amount of stress. We often think that that one fall, that one crash, is what’s going to break our bodies. The truth is, most injuries are the result of overuse—repetitive stress over a prolonged period—and while our body does a great job of adapting to the stress we place on it, its ability to repair itself diminishes the more time we spend in stress/pain.
So, now that OTH 2016 season is finished, show your body you care and make an appointment with a physical therapist. At Rausch Physical Therapy & Sports Performance, your PT will perform a biomechanical assessment to determine any new abnormal alignment patterns, soft tissue restrictions, or areas that you need to address this offseason to repair your body and prevent future injuries.
Conclusion
Stop allowing pain to determine how your body moves. While you may think you can live with “a little” hip pain, you may not realize that pain in one region of your body can lead to compensatory movement in another.
Think of it this way: think of how your derailleur cable on your bike can begin to stretch. This affects how your bike can shift, but you tell yourself you can live with that. But that small sound you hear from your chain grinding against the cassette means you’re slowly wearing down your chain, until one day—it breaks.
The moral of the story here is to listen to your body’s signs that your internal drive train is breaking down, and get it fixed.
 About Sean Swopes, PT, DPT, CSCS
About Sean Swopes, PT, DPT, CSCS
sean@rauschpt.net
Sean Swopes, DPT is the “Mountain Biking-PT” at Rausch Physical Therapy & Sports Performance. He is also a certified Strength and Conditioning Specialist. As a physical therapist, Sean’s goal is to help his patients understand their musculoskeletal impairments and work together to improve them.









 About Sean Swopes, PT, DPT, CSCS
About Sean Swopes, PT, DPT, CSCS


