Bursitis, a painful inflammation of the fluid-filled sacs cushioning our joints, can impact mobility. This common condition often affects major joints like the shoulders, elbows, and knees, making daily tasks a challenge for many people. This guide will help you manage and overcome bursitis, allowing you to regain comfort and return to your routine.
While rest and over-the-counter remedies can help ease flare-ups, true recovery often requires a tailored approach that addresses the root cause. Physical therapy is one of the most effective treatments, helping to strengthen surrounding muscles, improve joint flexibility, and prevent future inflammation. By learning the right movements and exercises under professional guidance, patients not only find relief but also regain the confidence to return to their daily activities without fear of recurring pain.
Bursitis is inflammation or irritation of a bursa sac. You have these sacs all over your body. They’re filled with fluid that eases rubbing and friction between tissues such as bones, muscles, tendons, and skin. Bursitis is common around major joints such as your shoulder, elbow, hip, or knee.
Bursitis is common in adults, especially after age 40.
It’s usually caused by repeated pressure on an area or by using a joint too much. High-risk activities include gardening, raking, carpentry, shoveling, painting, scrubbing, playing tennis, golf, skiing, and throwing. You can also get bursitis by sitting or standing the wrong way for a long time at work or home, or by not stretching enough before you exercise. Sudden injury can sometimes cause bursitis.
As you age, your tendons aren’t able to handle stress as well. They’re less elastic and easier to tear.
If there’s a problem with the structure of a bone or joint (such as legs that are different lengths or arthritis in a joint), it can put more stress on a bursa, causing bursitis. Reactions to medications and stress or inflammation from other conditions, such as rheumatoid arthritis, gout, psoriatic arthritis, or thyroid disorders, may also raise your risk.
An infection, especially with Staphylococcus aureus bacteria, can sometimes cause bursitis.
Bursas are small sacs filled with fluid that help cushion your joints, bones, and muscles. Any bursa can become inflamed, but the most common places to have bursitis are in your shoulder, elbow, knee, hip, or foot.
Bursitis can happen suddenly, or it can be ongoing (chronic). When it comes on suddenly, it usually hurts to move your affected joint. With chronic bursitis, a bursa swells slowly, and you may or may not feel pain.
Sometimes, bursitis is caused by an infection. This is called septic bursitis, and it’s not as common. Your doctor will check to make sure you don’t have an infection.
Shoulder bursitis
Shoulder bursitis causes painful swelling in your shoulder that gets worse when you move it. This can be caused by an injury or bump. Some people’s shoulder bones are naturally shaped in a way that puts more pressure on the bursa. If your bones are shaped like this, you’re more likely to get shoulder bursitis.
Depending on how bad the swelling is, you might not be able to move your shoulder, a condition called frozen shoulder. If it hurts too much to move your shoulder, you should see your doctor. They can do tests to find out if it’s bursitis or a different problem. They might recommend physical therapy for your shoulder or other treatments.
Elbow bursitis
One of the most common places to get bursitis is the pointy part of your elbow. If you have elbow bursitis, the bottom of your elbow will be swollen, red, and painful, with pain that gets worse when you bend it. Because of the swelling, it can look like there’s a small ball under your skin. If the ball gets bigger, it can make it harder to move your elbow.
Leaning on your elbows a lot can lead to elbow bursitis. Plumbers, electricians, HVAC technicians, and other people who have to crawl into tight spaces for work are more likely to put pressure on their elbows as they do their jobs. This kind of bursitis is also called “students’ elbow” because many people lean on their elbows when they sit at a desk to write or use a computer.
Injuries or bumps can also cause elbow bursitis. You might not remember the injury because it can take at least a week for bursitis to start. Doctors don’t understand why, but people who get dialysis for kidney problems are more likely to get elbow bursitis.
You can wrap an elastic bandage around your elbow or wear elbow pads to help ease your pain. If you do work that puts pressure on your elbows, wearing elbow pads or using a padded mat can help you avoid bursitis.
Knee bursitis
There are many different parts of your knee that can get bursitis, including near your kneecap or on the inside of your knee. If your bursitis is in your kneecap, it’s more likely to be caused by an infection.
When you have bursitis, it often hurts to move or put pressure on your knee, and it can hurt if someone else touches it. Your knee might also feel warmer than the rest of your body, and it sometimes looks swollen or red.
Sometimes, knee bursitis comes on suddenly after an injury or bump to your knee. More often, it’s caused by pressure on your knee joints over time, and the pain comes on slowly. Runners and people who kneel on the ground for work, such as landscapers, gardeners, and plumbers, are more likely to get knee bursitis.
If you do these kinds of work, you should wear knee pads or use a padded cushion or board under your knees and take as many breaks as you can. Try not to squat or bend your knees for too long. Stretching your hamstrings and other muscles before you exercise can help prevent knee bursitis.
People who fall a lot, such as wrestlers and people who play sports like football, are also more likely to get knee bursitis because they are more likely to bump or land on their knees.
Your doctor will look at both your knees, even if only one knee hurts, to compare them to each other and figure out what’s wrong. They might tell you to wear a knee brace or wrap to help you heal and protect your knees in the future. Putting your knee up on a pillow can help the swelling go down.
Hip bursitis
You can get bursitis in the bony part of your hip that sticks out near your waist. If you have this kind of bursitis, you might feel pain in your hip or outer thigh. You can also get bursitis on the inside of your hip, which causes pain in your hip, crotch, or groin.
You might not see any swelling if you have bursitis in your hip, but it can be painful. At first, the pain often feels sharp, and then turns into an ache that spreads out across your hip. It might hurt more when you lay on your hip, walk up the stairs, squat, or stand up from sitting down.
You are more likely to get this kind of bursitis if you have problems with your back or hips, if you’ve had hip replacement surgery, or if you were born with one leg that’s a little shorter than the other. Exercises such as running, riding a bike, or climbing up stairs can irritate it. You have a bigger risk of getting hip bursitis if you have a job where you have to move heavy things or stand up for long periods (for example if you’re a cashier, warehouse worker, or server).
If you have hip bursitis, your doctor might tell you to walk with a cane or use crutches while it heals. They might watch you walk, sit, and stand, or even videotape you. This will help them teach you less painful ways of moving around or standing.
Foot bursitis
There are 33 joints in your feet, and many of these joints have bursa sacs to protect them. You can get bursitis in your feet if any of these bursa sacs get irritated. You might have bursitis around your Achilles tendon in the back of your foot, near your heel, in the ball of your foot, at the base of your toes, or in between the outside of your little toe and your ankle.
If you have foot bursitis, your foot might feel swollen, stiff, or painful. The pain might get worse when you walk, run, or stand on your tip-toes.
High heels and shoes that squish your feet or don’t fit you well can lead to bursitis. Athletes, dancers, and runners are more likely to get foot bursitis.
Wearing supportive shoes that fit you well and stretching your feet and legs before you exercise can help prevent bursitis.
If you have foot bursitis, your doctor might tell you to go to a podiatrist. A podiatrist is a doctor who takes care of feet and ankles. They might give you a piece of foam or plastic called an orthotic to put in your shoe to cushion your foot.
Other types of bursitis
You have about 150 bursas throughout your body. It’s not as common, but you can get bursitis in any of these bursas. Some other types of bursitis are:
Pain is the most common symptom of bursitis. It might build up slowly or be sudden and severe, especially if you have calcium deposits in the area. You’ll probably feel it when you stretch or extend the joint, and you may have a limited range of motion even without pain.
Your joint might also be:
Call your doctor if you have:
- Fever (over 102 F or 38.89 C)
- Swelling, redness, and warmth in the area
- General illness or more than one area that hurts
- Trouble moving the joint
- Pain that lasts longer than 2 weeks
These could be signs of an infection or another problem that needs medical care right away.
You can’t always prevent bursitis, but some steps can lower your risk.
- Use cushions or pads when you’re resting a joint on a hard surface (for example, if you’re kneeling or sitting).
- If you play sports, mix things up so you don’t make the same motions all the time. Warm up and stretch before you play, and always use proper form.
- Start slowly and easily when you’re trying a new exercise or sport. As you build strength, you can use more force and do the motion more often.
- Don’t sit still for a long time.
- Take breaks often when you’re making the same motions over and over again.
- Maintain good posture all day.
- Hip bursitis can come from having one leg longer than the other. An orthotic shoe insert can help.
- Keep a healthy body weight.
- If something hurts, stop doing it and check with your doctor.
Your doctor will ask about your symptoms and do a physical exam to see if the joint is swollen. You might also have tests including:
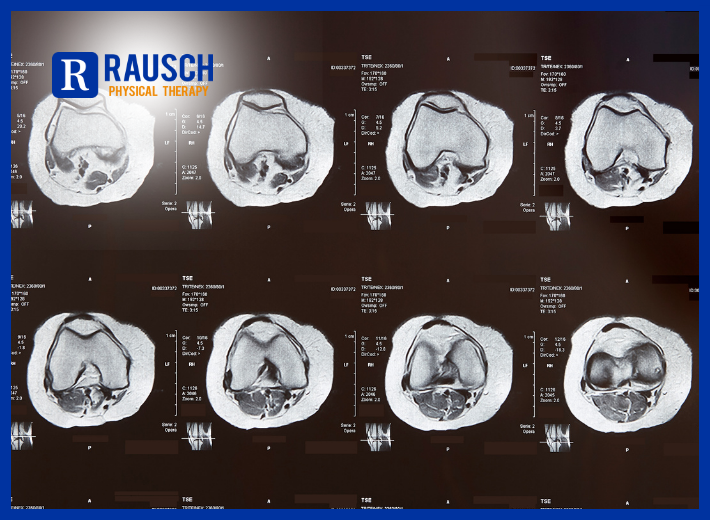
- Imaging tests. X-rays can rule out other problems that might be causing pain. MRI and ultrasound give your doctor an image of your joint.
- Lab tests. Your doctor might use a needle to take a bit of fluid from your bursa and test it for signs of infection.
Bursitis usually gets better on its own after a few weeks of resting the affected area. Try not to put pressure on it, and avoid activities that make the pain worse.
You can take medicine such as ibuprofen or naproxen sodium to lower the swelling and help with pain. Your doctor might give you this medicine in cream or lotion form.
See your doctor if you don’t feel better after resting the affected area. Call your doctor right away if you can’t move the joint at all or the area around it is very swollen or red. If you have a fever or there’s a rash or bruise on the area, you should see a doctor—these are signs that your bursitis might be caused by an infection.
Your doctor will do an exam to make sure it’s bursitis and not something else. They might have you bend or move the affected joint, or ask you to move around or walk. This helps them figure out which bursa is inflamed, and suggest exercises to help you heal. They might also do blood tests or imaging, such as an ultrasound or MRI, to get more information.
If your doctor thinks an infection could be causing your bursitis, they might take some fluid out using a small needle, and then test the fluid for bacteria. Your doctor will give you antibiotics to take at home if you have an infection. It’s rare, but you might need to stay in the hospital and get antibiotics through an IV, especially if you have immune system problems or if the infection is very bad.
Your doctor might give you steroids, a medicine that works quickly to lower inflammation and pain. They might prescribe steroid pills to take at home or use a small needle to inject steroids or pain medicine into the irritated area. Doctors disagree about whether steroid shots are helpful.
Depending on where your bursitis is, your doctor might tell you to use a cane, crutches or a brace, elastic bandage, or split.
Physical therapy can help you strengthen muscles and increase your joint’s range of motion. Your physical therapist might also teach you exercises for your core (the muscles in your back and belly that hold you up). A doctor or physical therapist can show you ways of sitting, standing, and moving that help bursitis get better or stop it from happening again.
It’s rare, but you might need surgery if other treatments aren’t helping.
Here are some things you can do to help your bursitis get better:
- Rest. Rest the area as much as you can, and avoid doing anything that makes the pain worse.
- Ice. Put an ice pack or cold compress on the area to help the swelling go down. After the first 2 days of icing it, you can also use a heating pad, hot water bottle, or heat pack, or take a hot bath or shower.
- Support the joint. Use a brace, ace bandage/elastic band, or splint to cushion the joint.
- Elevate it. Put the affected joint up on pillows.
- Cushioning. Pad the affected area and avoid hard surfaces. For example, use knee pads or a padded mat if you need to kneel down for work, or sit on a donut-shaped pillow or padded cushion instead of on the floor.
- Stretching and exercise. Stretch before exercising. Doing exercises that strengthen your core muscles and make you more flexible can help some kinds of bursitis.
- Posture. Use good posture and body mechanics. A doctor or physical therapist can help you learn ways to move, sit, and lift that are easy on your body and won’t irritate your joints.
- Massage. Massaging the area can help, but you should check with your doctor to make sure your bursitis isn’t caused by an infection before you massage it.
- Avoid repetitive movements, pressure, and heavy lifting. If possible, avoid putting pressure on the area, don’t lift heavy things, and try not to do the same motions over and over. If you can’t avoid this, take as many breaks as you can. Ask your doctor for a note if you need to miss work or make changes to the kind of work you do—for example, sitting on a padded chair instead of standing.

Don’t let bursitis continue to sideline you. At Rausch Physical Therapy, our expert team specializes in personalized bursitis care designed to restore strength, reduce inflammation, and get you back to doing what you love. Call us today at 949-276-5401 to schedule your appointment, and follow us on Instagram @rauschpt for more tips, insights, and recovery inspiration.
Reference: [https://www.webmd.com/pain-management/arthritis-bursitis]





 3. Snack well
3. Snack well 5. Drink up
5. Drink up Let experience be your guide
Let experience be your guide








 How Do You Prevent Bursitis?
How Do You Prevent Bursitis?


 5. Get a Massage
5. Get a Massage


 Struggling with discomfort or limited movement due to tight hips? Don’t let it hold you back! Call our physical therapy center today at 949-276-5401 and take the first step towards a more comfortable, active life. Our comprehensive approach helps you heal faster, move better, and stay stronger for the long run.
Struggling with discomfort or limited movement due to tight hips? Don’t let it hold you back! Call our physical therapy center today at 949-276-5401 and take the first step towards a more comfortable, active life. Our comprehensive approach helps you heal faster, move better, and stay stronger for the long run. 


 Visit Us: 25252 McIntyre St, Ste A, Laguna Hills, CA
Visit Us: 25252 McIntyre St, Ste A, Laguna Hills, CA Fort Fitness:
Fort Fitness:  Book with Rausch PT:
Book with Rausch PT: 
 Hand Fractures
Hand Fractures


 Light Exercise
Light Exercise Preventing DOMS
Preventing DOMS



